How outsourcing is helping boost telehealth services
Given the choice, there’s no doubt most of us would prefer to live in a world where we had never heard of COVID-19. A world in which more than 7 million people had not succumbed to the disease1. A world that had not endured one of the worst job crises since the Great Depression2. A world in which the global prevalence of anxiety and depression did not soar by 25% in one year3. It is more than four years since the first case of coronavirus was recorded and no one has forgotten the devastating toll the pandemic took on countless nations, communities and individuals.

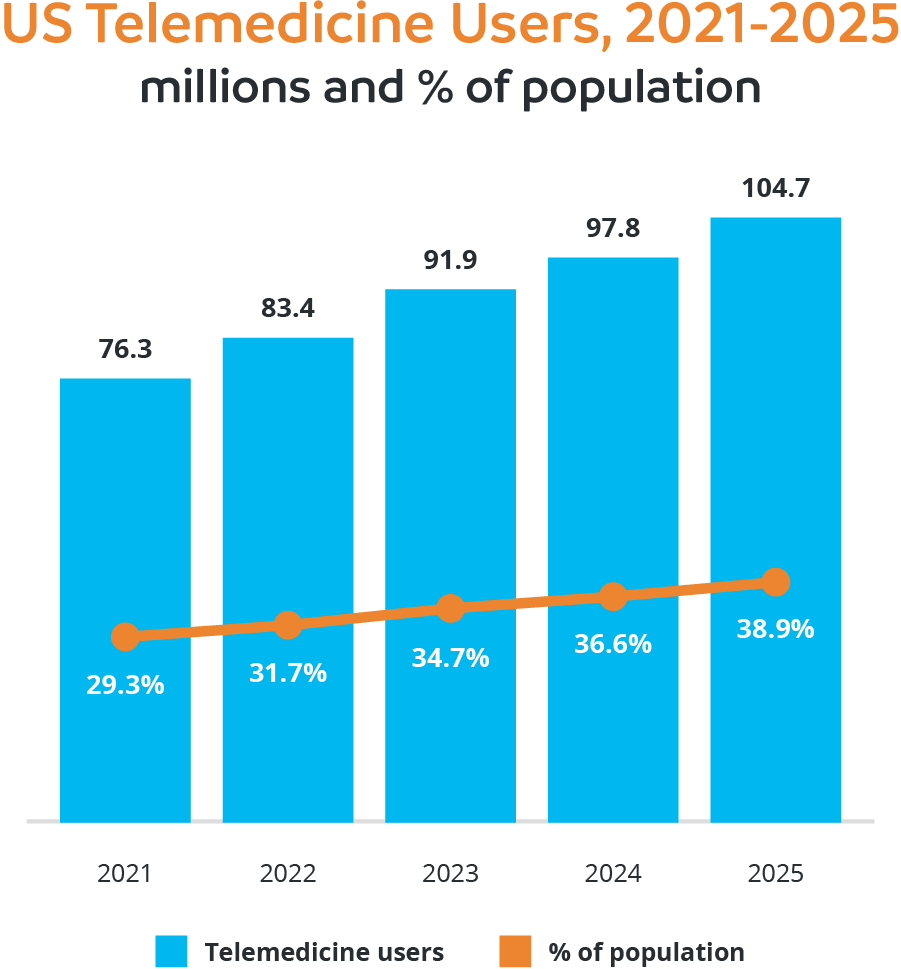
Nowhere was that pain felt more than in the health sector, which is why it is somewhat ironic that one of the few positive side effects to emerge from that period has been the rise of telehealth. While many hospitals and health practices provided some form of telehealth or telemedicine services prior to the pandemic, it has been estimated they accounted for less than 1% of outpatient encounters in early 20204. Then came the new world of social distancing and lockdowns and the figure soared to more than 13% in the first six months of the pandemic and Medicare telehealth utilization had a remarkable 63-fold increase5.
As the world grappled with the impact of coronavirus, the U.S. Congress removed a multitude of telehealth regulations to make it easier for people to access healthcare virtually and both the public and clinicians clearly liked the new approach. An American Medical Association study has found more than 80% of physicians believe patients have better access to care since using telehealth6, while 94% of patients who have had a telemedicine encounter want to access similar support in the future7.
‘House calls’ from doctors are once again surging but rather than the traditional knock on the door, they are pinging their patients’ smartphones and consulting via online conferencing platforms. Technology will never fully replace face-to-face consultations but telehealth is undoubtedly here to stay and that is inspiring a growing number of hospital and healthcare providers to seek support from outsourcing providers that specialize in telehealth services.
Given such demand, this article will showcase the benefits of telehealth, highlight potential hurdles, explain how outsourcing can boost service offerings and outline key steps for choosing a quality outsourcing partner.
Content guide
What are telehealth services?
Telehealth services are the use of virtual and digital technologies to provide healthcare, support and information to patients in remote settings. Such technologies can include computers, mobile devices and video conferencing and allow clinicians to deliver consultations when a physical examination is not required. The American Hospital Association has declared that it “supports the expansion of patient access created by hospitals’ efforts to deliver high quality and innovative telehealth services”8.
What is telehealth outsourcing?
Telehealth outsourcing is the practice of hospitals and healthcare providers partnering with external agencies or individuals to boost their telehealth services. This can include the outsourcing providers taking care of parts of their telehealth operations including remote patient monitoring, telemedicine consultations and administrative tasks.
What are the types of telehealth services?
The number of telehealth services available for patients and clinicians is expanding as technology evolves.
- Telemedicine: remember the days of needing to physically visit a medical practice for even the most minor of consultations? Telemedicine has changed the game by allowing the remote diagnosis and treatment of patients using telecommunications technology. Options range from video consultations and digital transmission of medical imaging to remote medical diagnosis and evaluations, with the most common platforms including phone, text message and video chat.
- Telepsychiatry: telehealth is playing a vital role in helping deliver convenient and affordable mental health services, which is all the more important given the increasing demand for care. Telepsychiatry allows patients who cannot access face-to-face therapy the opportunity to engage with specialist clinicians via video, phone or SMS chats and is particularly welcomed by rural communities where such services are often lacking.
- Telehealth nursing: the pandemic created a situation where hospitals were forced to limit nurse-patient interactions but fortunately the healthcare professionals were able to use technology to bridge the gap. This service has extended into the post-COVID world, with remote patient monitoring tools and wearable devices meaning nurses are not required to visit someone’s room every time they need to check health indicators. This is also helping hospitals alleviate labor shortages.
- Specialist advice: telehealth is not only opening lines of communication between clinicians and patients but allowing hospitals and healthcare providers to easily seek advice from fellow experts. Primary care providers can instantly provide specialists with the likes of consultation notes, medical histories, test results and X-rays, increasing the response time and quality of care provided to patients.
What are the benefits of telehealth?
The growing popularity of telehealth is on the back of an extensive list of benefits for patients and clinicians.
- Comfort and convenience: life is tough enough when battling illness or injury without needing to drive to a doctor’s office or clinic. Instead of finding a car park and being forced to bide time in a waiting room, many patients can receive the same consultative care from the comfort of their own bed or couch. Virtual visits can also more easily slot into someone’s schedule and even reduce the need to take time off work or arrange childcare.
- Control of infectious illnesses: telehealth services were crucial in helping stop the spread of COVID-19 and can continue to play a similar role in relation to flu and similar infectious diseases. The ability of doctors to use virtual consultations to pre-screen patients saves sick people from needing to visit medical clinics and reduces exposure to other people’s germs, which is especially vital for the chronically ill, pregnant, elderly or immunocompromised.
- Chronic condition management: people battling chronic conditions endure what must seem like a never-ending stream of medical appointments and hospital visits. Telehealth is easing that burden by allowing them to more easily connect with primary care practitioners that specialize in their area of need and reducing the need to continually travel across suburbs, cities and even states to access care.
- More resources for critical patients: hospitals and health practices often face the dilemma of needing to divert resources from critical patients to process or consult with people with less urgent concerns. The opportunity to manage such patients via tools such as video conferencing is welcome relief for busy clinicians, let alone people requiring more specialist and personalized attention.
- More care for more people: everyone knows the feeling of walking into a clinical waiting room to find a seemingly endless queue of people seeking care. Now imagine many of those people can be seen quickly and seamless without even needing to visit the clinic. That becomes a reality with telehealth, with doctors and nurses able to see more people both online and in person.
What are the challenges with telehealth?
For its many benefits, there are a handful of issues that telehealth users need to consider.
- Connectivity challenges: many telehealth services rely on access to high-speed broadband internet, which is not guaranteed in some geographic locations and of particular concern for rural patients. Buffering videos may be annoying on YouTube but they can be devastating for people desperate to communicate with their clinicians.
- Lack of technical expertise: hospitals and health providers have a responsibility to ensure clinicians and other staff have the knowledge and skills to navigate the technological aspects of utilizing telehealth services. This may require an investment in training and resources but the benefits will be significant. It is also important to be understanding and supportive of patients who struggle with using telehealth platforms, particularly the elderly and those who do not use technology daily.
- Patient confidentiality: health consultations typically require the transferral of sensitive patient data and doing so via video link can be of concern for patients. There is an onus on hospitals and health providers to ensure that such information is treated with the utmost care and using a secured communication channel and partnering with HIPAA-compliant partners can boost patients’ confidence.
What are the benefits of telehealth outsourcing?
Outsourcing telehealth services can provide significant benefits to healthcare organizations.
- Sustainable growth: in the wake of the pandemic, many hospitals and health providers are focused on allocating resources in a fiscally responsible manner to ensure long-term and sustainable growth. Outsourcing telehealth services can significantly reduce operational expenses as it eliminates the need to pay for potentially costly in-house telehealth infrastructure and staff. Outsourcing also allows health organizations to only pay for certain telehealth services when they are required.
- Specialist knowledge: delivering quality telehealth care requires a variety of skill sets that are not always readily available within a hospital or health practice. From knowledge of technology platforms and regulatory compliance to the nuances of virtual communication, quality outsourcing providers that specialize in telehealth have a deep understanding of such areas and can elevate a service’s telehealth offering without needing to develop in-house expertise.
- Scalability: outsourcing has long been known for allowing organizations to seamlessly scale their operations based on demand and it is no different with telehealth. Given the uncertain nature of healthcare where hospitals and practices routinely deal with fluctuations in patient volume, outsourcing providers can quickly adjust to changing circumstances and allow their health partners to deliver a responsive telehealth service.
- Focus on core services: as a relatively new concept, telehealth has forced many healthcare providers to dedicate resources to the field at the expense of their primary services. By assigning telehealth-related tasks and management to outsourcing providers, hospitals and health practices can spend more time and energy on their core mission of delivering high quality healthcare services to patients.
- Less administration: outsourcing need not stop at telehealth services. Anyone who has worked in a healthcare organization will be familiar with the number of administrative tasks that steal precious resources away from frontline services. From medical billing and transcription to payroll services and appointment scheduling, many outsourcing providers are equally adept at streamlining such time-consuming and repetitive tasks as they are at managing telehealth services.
How do you choose an outsourced telehealth provider?
Partnering with an outsourcing telehealth provider is the easy decision. The true challenge is identifying one that has the knowledge, skills and people to enhance your offering. These tips will go a long way to achieving that.
- Proven track record: do your research to find a provider that not only has extensive experience in the outsourcing sector but an intimate knowledge of the healthcare space. Seek testimonials from other clients and review case studies that show how they have performed in the telehealth space.
- Quality technology: technology lies at the heart of telehealth, which is why it is essential to ensure your outsourcing partner is committed to providing best-practice platforms and infrastructure. It will quickly become clear which providers deliver on this front.
- HIPAA compliance: when it comes to non-negotiables, teaming with an outsourcing provider fully invested in HIPAA compliance is near the top of the list. The security and confidentiality of telehealth patients’ personal and health information is crucial and your outsourcing provider should proactively demonstrate their commitment to maintaining HIPAA standards.
- Value for money: be mindful that what you see in an outsourcing provider’s pitch is not always what you get. To ensure your outsourced telehealth strategy makes great financial sense, choose a provider that is upfront about its costs and avoids the ‘hidden charges’ we all dread. Working with a provider in an outsourcing destination such as the Philippines can reduce labor costs by up to 70%.
Summary
At the peak of the pandemic, a leading news website declared that “telehealth may become (a) big part of (the) new normal”9. Four years on and that has proven to be the case as an increasing number of hospitals and health services strengthen their offerings in the area to meet the expectations of both patients and clinicians. It is no easy task though and it is reassuring to know they do not have to go it alone given help is at hand in the form of outsourced telehealth providers.
At a time of significant financial pressures, effective revenue cycle management (RCM) has never been more important for healthcare executives. Discover how outsourcing is helping hospitals and health practices optimize their RCM practices by tackling the likes of patient registration, insurance verification and claims submission.
Reference:
[1] COVID - Coronavirus Statistics - Worldometer (worldometers.info)
[2] COVID - Coronavirus Statistics - Worldometer (worldometers.info)
[3] COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide (who.int)
[4] Outpatient telehealth use soared early in the COVID-19 pandemic but has since receded - Peterson-KFF Health System Tracker
[5] It’s Time to Cement Telehealth’s Place in U.S. Health Care (hbr.org)
[6] Telehealth resource center: Research findings | American Medical Association (ama-assn.org)
[7] 2022 U.S. Telehealth Satisfaction Study | J.D. Power (jdpower.com)
[8] Fact Sheet: Telehealth | AHA
[9] The doctor is online: Telehealth may become big part of new normal - VTDigger
Popular posts
Browse by topic
- Accounting
- Accounting & Finance
- All Industries
- Banking
- BPO/RPO/HRO
- Communication
- CSR & ESG
- Customer & Client Acquisition
- Customer Experience
- Cybersecurity
- Cybersecurity & Compliance
- Data Management
- Digital Operations
- Digital Transformation
- eCommerce
- Education
- Employee Engagement
- Engineering & Construction
- Financial Services
- Healthcare
- Hospitality and tourism
- HR & Recruitment
- Information Technology
- Insurance
- Legal Services
- Logistics
- Offshoring & Outsourcing
- Outsourcing
- Professional Services
- Real Estate
- Retail & eCommerce
- Startups
- Talent Acquisition and Retention
- Technology
- Trends & Guides
- Workforce Integration
Sign up for the offshoring eCourse
12 in-depth and educational modules delivered via email – for free
Related Posts
Finding value in partnerships: evaluating offshore providers for healthcare cost management
Academic journal The Conversation did not hold its punches when it recently turned its attention to a crisis engulfing the healthcare sector. Beneath..
How to improve patient experience in healthcare
It says a lot about the economic realities of modern-day health care that one of America’s most prestigious learning institutions has a course..
Is offshore staffing the key to data compliance?
With entire websites dedicated to exposing businesses daily that have been hacked or have had their data breached daily, it’s no wonder why data..
